That shooting pain down your leg that makes you catch your breath, the tingling that won't go away, or the ache that's keeping you awake at night - if this sounds familiar, you're likely dealing with sciatica. As physiotherapists, we see patients with sciatica regularly, and one of the first things they ask is: "What can I actually do about this pain?"
The good news is that most sciatica responds very well to the right approach. While it can feel overwhelming when you're in pain, understanding what sciatica is, what triggers it, and most importantly, what you can do to help yourself can make a significant difference to your recovery.
What Does Sciatic Pain Feel Like?
Sciatica isn't just "back pain that goes down your leg." Patients describe sciatica pain in very specific ways that help us understand what's happening:
"Like an electric current running down my leg"
"A hot wire from my back to my foot"
"Sharp shooting pain that takes my breath away"
"Burning sensation that travels down my thigh"
"Tingling and numbness, like my leg's gone to sleep"
The pain typically follows the path of your sciatic nerve - from your lower back, through your buttock, down the back or side of your thigh, and sometimes all the way to your foot. It's usually worse on one side, though it can affect both legs.
Not everyone experiences sciatica as sharp or burning pain — for some, it presents as a persistent mild ache in the buttock, thigh, or calf.
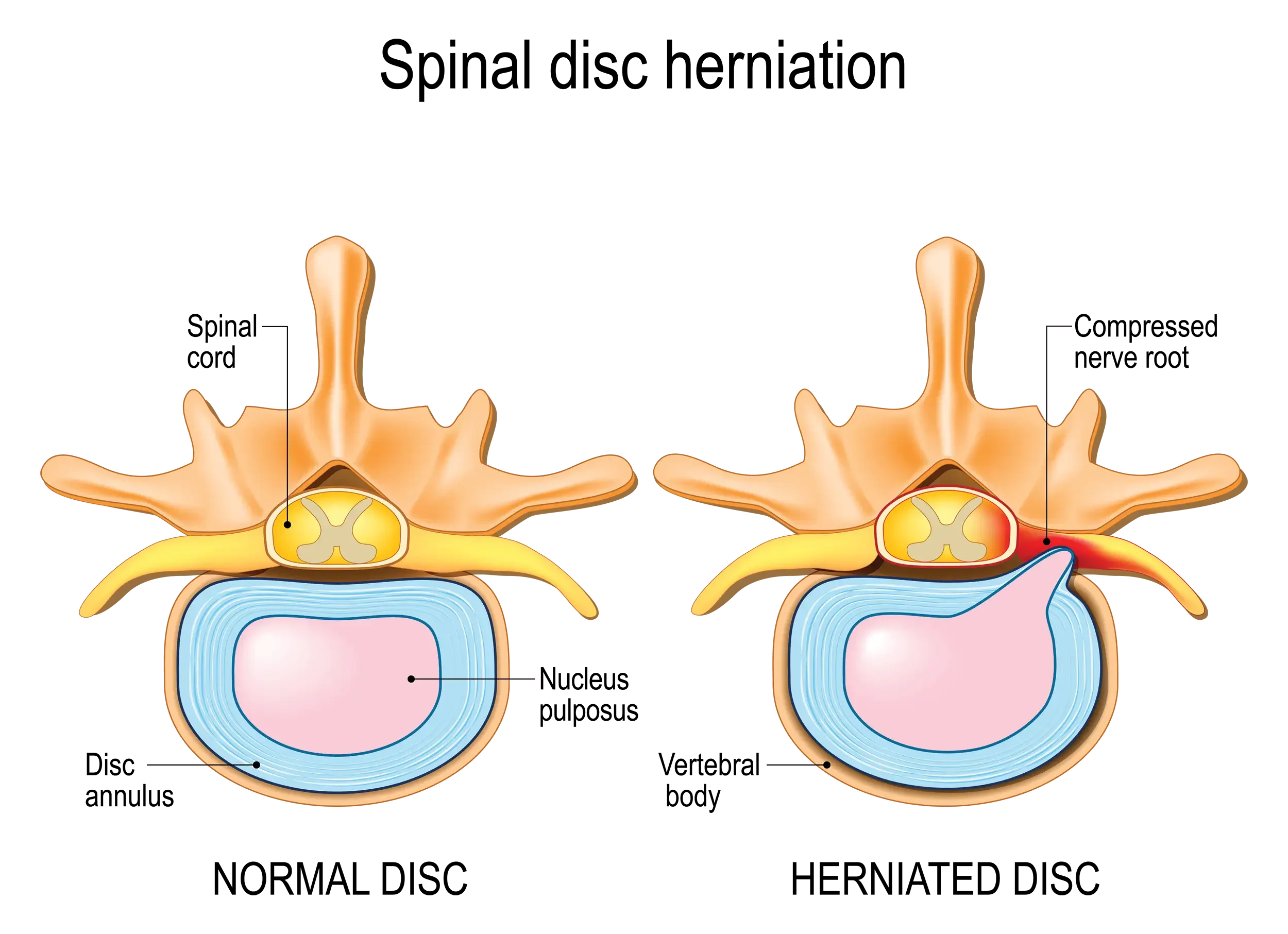
Understanding the Confusion: Is a Slipped Disc the Same as a Herniated Disc?
Before we dive into treatment, let's clear up a common confusion that causes unnecessary worry for many sciatica patients.
The simple answer: Yes, they're the same thing. Whether you've been told you have a "slipped disc," "herniated disc," "prolapsed disc," or "ruptured disc," these terms all describe different severities of the same issue.
Your spinal discs haven't actually "slipped" anywhere - think of them more like jam donuts. The tough outer ring can develop a weakness, allowing some of the soft inner material to bulge out or leak through. When this presses on the sciatic nerve, it can cause the pain that travels down your leg.
““I reassure patients that regardless of which term their previous doctor used, what matters is how we can help them recover. The treatment approach is the same whether you call it slipped, herniated, or prolapsed.””
What Triggers Sciatica Pain?
Understanding your triggers helps you manage symptoms and prevent flare-ups:
Common Triggers Include:
Sitting for long periods - especially in poor posture
Bending forward - particularly first thing in the morning
Coughing or sneezing - increases pressure in your spine
Lifting or twisting - especially when combined
Getting out of bed - after lying still for hours
Why Sciatica Is Often Worse at Night
Many patients find their sciatica pain intensifies during the night or early morning. This happens because:
Lying flat can sometimes increase pressure on the affected nerve
Reduced movement during sleep can cause stiffness
Inflammation tends to build up overnight
Muscle tension accumulates from the day
Immediate Steps You Can Take for Sciatica Relief
When sciatica strikes, here's what our physiotherapists recommend you do right away:
1. Keep Moving (Gently)
Contrary to what many people think, complete bed rest usually makes sciatica worse. Gentle movement helps reduce inflammation and prevents stiffness.
Try these movements:
Walking - even just 5-10 minutes if that's all you can manage
Gentle marching on the spot - when walking is too painful
Supported standing - holding onto a chair or wall
2. Find Your Comfortable Positions & Personal Preferences
Different positions work for different people, but these often provide relief:
For sitting:
Use a small rolled up towel behind your lower back
Keep your feet flat on the floor
Avoid low, soft chairs that make you slouch
For lying down:
Lie on your back with a pillow under your knees
Or lie on your side with a pillow between your knees and a small rolled towel rolled up and place between the ribs and the top of the pelvis.
Some people find lying on their stomach helpful
For standing:
Avoid standing in one position for too long
Shift your weight from foot to foot
Use a small footstool to rest one foot if standing for a while
3. Simple Stretch & Pain Relief Techniques
Heat or Cold:
Ice for the first 48-72 hours if there's acute inflammation
Heat after the initial phase to relax muscles
Alternating heat and cold can sometimes work well
Gentle Stretches (only if comfortable):
Knee to chest - lying on your back, gently pull one knee toward your chest
Gentle hip stretches can help if muscle tension is contributing
Cat-cow movements on hands and knees if you can get into this position
Some patients also find gentle massage helpful, particularly when muscle tension is contributing to their discomfort. While it won’t fix the underlying nerve irritation, it can provide short-term relief and relaxation.
"The key with sciatica is listening to your body. If a movement or position makes your leg pain worse, avoid it. If it reduces the leg pain, even if it slightly increases back pain, that's usually a good sign." – Phil Harris - spinal physio.
When to Seek Professional Help for Sciatica
While many cases of sciatica improve with self-care, certain situations require prompt professional assessment:
Seek Help Within a Few Days If:
Pain isn't improving with basic self-care measures
You're unable to find any comfortable positions
The pain is preventing you from sleeping
You're struggling with daily activities
Seek Urgent Help If You Experience:
Loss of bladder or bowel control
Severe weakness in your leg or foot
Numbness around your genital area
Progressive neurological symptoms
Severe pain following an accident
These "red flag" symptoms are rare but need immediate medical attention.
How Physiotherapy Can Help Fix Sciatica
Professional physiotherapy treatment for sciatica focuses on several key areas:
Reducing Nerve Irritation
Manual therapy techniques to improve spinal movement
Nerve mobilisation exercises to reduce sensitivity
Postural correction to reduce ongoing pressure
Addressing Root Causes
Strengthening weak muscles that may be contributing
Improving flexibility in tight areas
Correcting movement patterns that might be aggravating the problem
Education and Self-Management
Understanding your condition and what to expect
Learning which activities to modify and which are safe
Developing a long-term prevention strategy
Having clear, accurate information about your condition helps reduce fear and gives you the confidence to keep moving and recover more effectively.
““Sciatica often responds really well to physiotherapy because we can address both the symptoms and the underlying factors that led to the problem. Most patients see significant improvement within 4-6 weeks with the right approach.””
What Exercise Is Good for Sciatica Pain?
Exercise is crucial for sciatica recovery, but the right exercises depend on your specific situation:
Early Phase (When Pain Is Severe):
Gentle walking as tolerated
Basic postural awareness exercises
Simple breathing exercises to help manage pain
As Pain Improves:
Core strengthening exercises
Hip flexibility work
Nerve gliding exercises (under professional guidance)
Prevention Phase:
Comprehensive strengthening program
Movement retraining for daily activities
Sport or activity-specific preparation if needed
How Long Does Sciatica Pain Last?
This varies significantly, but here's what research tells us:
Typical Timeline:
Acute phase: 1-2 weeks of severe symptoms
Improvement phase: 4-6 weeks of gradual improvement
Recovery phase: 8-12 weeks to near-normal function
Factors That Affect Recovery Time:
How quickly you start appropriate treatment
Whether you stay active within your limits
Your overall fitness and health
The specific cause of your sciatica
How well you follow professional advice
Case Study: Emma's Sciatica Recovery
Emma, a 38-year-old office worker, developed severe sciatica after lifting boxes during a house move. The pain shot from her lower back down to her ankle, making sitting at work almost impossible.
Week 1-2: Emma tried complete bed rest, which made her symptoms worse. She contacted our clinic when the pain wasn't improving.
Initial treatment focus:
Pain relief techniques and positioning advice
Gentle movement exercises
Workplace modifications for immediate relief
Week 3-6: As Emma's acute symptoms settled, treatment progressed to:
Specific strengthening exercises
Manual therapy to improve spinal movement
Gradual return to normal activities
Week 8-12: Emma focused on:
Comprehensive prevention program
Return to all normal activities including exercise
Long-term maintenance strategies
Outcome: Emma returned to full function and remained symptom-free at 6-month follow-up by maintaining her exercise programme and using proper lifting techniques.
How to Sit with Sciatica Pain
Since sitting often aggravates sciatica, here are specific strategies:
Chair Setup:
Lumbar support: Use a rolled towel
Feet flat: On the floor or on a footrest
Knees level: With or slightly below your hips
Avoid: Deep, soft sofas that make you slouch
Regular Movement:
Stand every 20- 30 minutes if possible
Gentle back extensions when you stand
Shift positions regularly while sitting
Consider a standing desk option if feasible
Alternative Positions:
Perching on a high stool
Kneeling chairs work well for some people if you have no knee issues.
Exercise ball for short periods (if comfortable)
How to Relieve Sciatica Pain in Pregnancy
Pregnancy-related sciatica requires special considerations:
Safe Relief Methods:
Prenatal yoga poses (with instructor guidance)
Swimming or water exercises
Pregnancy support belts
Heat therapy (avoiding overheating)
Positioning Help:
Pregnancy pillows for better sleep positioning
Avoid sleeping on your back after the first trimester
Side-lying with pillow support between knees
"Pregnancy sciatica often improves significantly after delivery, but we can still provide safe, effective treatment during pregnancy to help mothers stay comfortable and active." –Sarah Lawson - Spinal Physio
““Pregnancy sciatica often improves significantly after delivery, but we can still provide safe, effective treatment during pregnancy to help mothers stay comfortable and active.””
Red Flags: When Sciatica Needs Urgent Attention
While most sciatica isn't dangerous, certain symptoms require immediate medical assessment:
Emergency Symptoms:
Cauda equina syndrome signs: Loss of bladder/bowel control, saddle numbness
Severe progressive weakness: Inability to lift your foot or difficulty walking
Bilateral symptoms: Sciatica affecting both legs severely
Concerning Changes:
Rapidly worsening symptoms despite appropriate treatment
New neurological symptoms like significant numbness or weakness
Signs of infection like fever with back pain
The Best Treatment Approach for Sciatica
Research shows that the most effective treatment for sciatica combines:
Early, appropriate movement rather than bed rest
Professional assessment to identify specific contributing factors
Graduated exercise program tailored to your recovery stage
Education about the condition and self-management strategies
Manual therapy when appropriate
Pain management techniques to help you stay active
What Makes Treatment Successful:
Starting treatment early rather than waiting for it to "go away"
Staying active within your pain limits
Following professional guidance consistently
Addressing underlying factors like posture or fitness
Having realistic expectations about recovery timeline
Is Sciatica Curable?
The encouraging news is that most sciatica has an excellent prognosis:
Complete Recovery: 80-90% of people with sciatica recover completely within 6-12 weeks with appropriate treatment.
Good Improvement: Most others experience significant improvement that allows them to return to normal activities.
Chronic Cases: Only a small percentage develop long-term problems, usually when treatment is delayed or inappropriate.
Prevention: Learning proper movement patterns and maintaining fitness significantly reduces the risk of recurrence.
Taking Action on Sciatica & Back Pain: Your Next Steps
If you're dealing with sciatica pain:
Don't panic - most sciatica resolves well with appropriate care
Stay gently active - complete rest usually makes it worse
Try the positioning and movement advice outlined above
Seek professional help if symptoms aren't improving within a few days
Be patient - recovery takes time but is usually very successful
Remember, sciatica is common, treatable, and in most cases, completely recoverable. The key is taking the right steps early and getting professional guidance when needed.
““The most important thing I tell patients with sciatica is that this condition responds really well to treatment. Yes, it can be painful and concerning, but with the right approach, the vast majority of people make a full recovery.””
Ready to get help with your sciatica? Our experienced spinal physiotherapists can assess your specific situation and create a treatment plan to get you back to pain-free movement.